Periacetabular osteotomy (PAO)
What is a periacetabular osteotomy (PAO)?
Periacetabular osteotomy (or PAO for short) is a complex surgical procedure which involves reorienting the socket of the hip joint (acetabulum) to improve the mechanics of the hip. Breaking down the parts of the word into layman's terms: "Peri" means "around", "acetabular" refers to the hip socket, and "osteotomy" is the medical term for a procedure that cuts bone.
The procedure was developed in Bern, Switzerland with the first PAO performed by Reinhold Ganz in 1984. Since then, the technique has been modified to be less invasive and spread around the world as one of the most powerful techniques in hip preservation surgery.
Why is PAO Recommended?
It is most commonly performed to treat adolescent and adult hip dysplasia, a condition where the hip socket is too shallow and does not adequately cover the ball portion of the upper thigh bone (the femoral head). This lack of coverage means that the forces passing through the hip are concentrated on a small area of cartilage at the edge of the socket, resulting in pain, labral tears and an increased risk of developing arthritis over time. The surgery involves repositioning the hip socket to provide better coverage and stability, ultimately improving hip function and reducing pain.
PAO may also be recommended to treat acetabular retroversion, a form of dysplasia in which the socket is pointing backwards, instead of slightly forwards, leading to impingement (mechanical conflict) of the femur against the front wall of the socket.
PAO is typically recommended for patients who have ongoing hip pain, after they've already tried appropriate non-operative management such as physiotherapy for at least 3 months.
The typical age range of patients who may be suitable for PAO is between 15-40 years old. In select cases, patients slightly outside this range may also be good candidates. As PAO is a hip preservation procedure, some patients may not be suitable if there is already too much damage (arthritis) within the joint, seen on MRI or x-ray.
The goals of PAO are to relieve pain, restore function and hopefully prevent or delay the progression of arthritis within the joint.
Dr. Williams will carefully assess your individual case and recommend PAO if it is deemed the most appropriate course of action for your condition.

Dr Williams' Periacetabular Osteotomy (PAO) Surgical Technique
PAO is a complex, multi-step operation requiring thorough planning, in-depth understanding of a patient's three-dimensional pelvic anatomy and meticulous surgical technique.
Dr Williams has undertaken extensive further training in PAO surgery and performs this surgery regularly in both adults and teenagers, using a rectus and abductor muscle-sparing approach through a single oblique incision.
Set-up
The surgery takes 2-2.5 hours and is performed under general anaesthetic with the patient lying on their back on a radiolucent x-ray table. A foot bolster is positioned to allow the hip to be bent up at different stages of the operation. A urinary catheter is placed to empty the bladder in order to avoid injury. As well as a general anaesthetic, a nerve bock, spinal or epidural may also be performed to keep the patient comfortable.
Cell Saver technology is used to salvage as much of the inevitable blood loss during the procedure as possible. A patient's own blood is then filtered and re-transfused, to reduce the need for transfusion of donated blood.
Approach
The skin incision is approximately 10-15cm long and runs over the point of the hip in an oblique direction, parallel to the skin tension lines. The abdominal muscles (external oblique) are released off the crest of the pelvis and the main hip flexor muscle (iliacus) is elevated to expose the pelvic 'wing' on its internal surface. The pubic bone part of the pelvis is exposed with the hip bent right up to relax the hip flexor tendons, femoral nerve and vessels.
Osteotomies (bone cuts)
Once the pelvic bone is properly exposed and the muscles held out of the way, Dr Williams carefully performs the releasing cuts required to move the bone fragment. These cuts are performed with specially designed chisels as well as a saw and are guided by live intra-operative x-ray. 4 main osteotomies are performed in order: the pubic, the ischial, the iliac and the retroacetabular osteotomy.
Careful technique, including the use of live x-ray, is required whilst performing the bone cuts to avoid rare but potentially serious complications such as nerve injury or breaching into the hip socket.
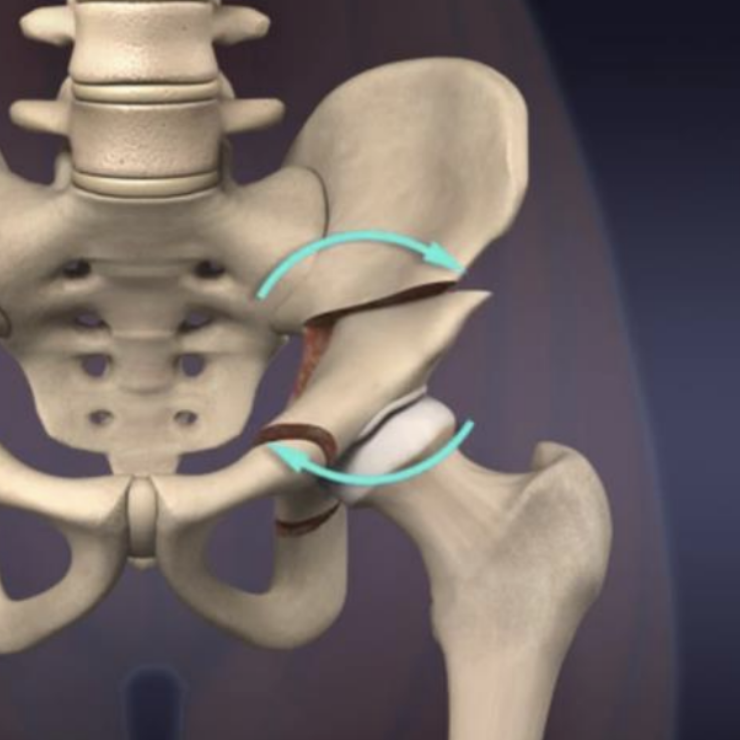
Socket repositioning
A large screw (known as a Schanz pin) and clamp are used to rotate the socket into a better position under intra-operative x-ray guidance. The hip should be well-covered to support the forces passing through the ball, but not over-covered, which could lead to impingement.
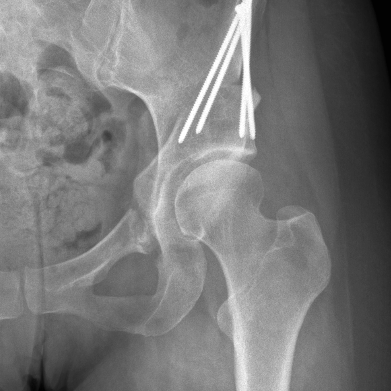
Determining the correct position is the most important part of the operation and so extra time is spent getting this right before the fragment is fixed in place with 3-5 stainless steel screws of 3.5mm diameter.
Closure
A wound infusion catheter is placed to deliver local anaesthetic deep into the surgical field for several days. The muscles are repaired back to the pelvic crest with strong dissolvable sutures. The skin is closed in multiple layers, with the final layer being a dissolvable running suture just below the skin. The outer surface of the wound is then sealed with glue and a waterproof dressing is applied, to be left on for 2 weeks.
Periacetabular osteotomy (PAO) recovery
Like most orthopaedic surgeries, full recovery following a PAO can take up to 12 months. That being said, you will be steadily improving throughout that time and usually mobile without any crutches by 8-10 weeks. Younger patients (teenagers) tend to heal faster and are often walking unaided by 6 or 7 weeks.
Patients usually stay in hospital for 3-6 nights following their surgery. Some common (and expected) issues during the first few days include lightheadedness, nausea, pain at the surgical site and difficulty mobilising. Dr Williams and his team will see you to troubleshoot any of these issues and the acute pain team will also see you regularly to keep you as comfortable as possible.
The physiotherapists will give you instructions on exercises you can do in bed, teach you how to get in and out of bed on your own and get you moving with crutches. For the first 4 weeks, you can only put 20% of your weight through the operated leg. Dr Williams is usually happy for you to build this up to 50% for weeks 4-6 and then 100% from week 6, if the x-ray shows good signs of healing.
One thing to be aware of is that you will not be able to lift the leg very easily for the first 4-6 weeks after surgery, which can make some movements quite challenging such as repositioning the leg in bed, getting in and out of bed or into a car. This is due to a normal part of the surgery that involves elevating the hip flexor muscle off the bone, which then takes time to heal. The physios will demonstrate ‘work arounds’ for this in hospital such as using the other leg, a crutch or a specially designed leg-lifter to help.
After discharge from hospital, you will carry out exercises at home until Dr Williams sees you at 2 weeks post-op to check your wound.
After the 2 week check, formal physiotherapy can begin, although is very gentle for the first 6 weeks. Dr Williams will liaise with your physiotherapist to provide some evidence-based rehabilitation guidelines, as some physios may not yet be familiar with the procedure.
Periacetabular osteotomy (PAO) FAQs
Recommended resources
If you would like to read more about the periacetabular procedure, Dr Williams recommends the following websites:
- International Hip Dysplasia Institute (includes a nice animation of the surgery)
- miles4hips.org. (A good patient-centred resource with many patient stories)
- OrthoInfo from the American Academy of Orthopaedic Surgery (good general information)